These notes were taken at the 2014.Dec.18 New England Complex Systems Institute Salon focused on Ebola. Sam, Willow, Yaneer contributed to this write-up, and 20 people were in attendance. We hope you’ll join us in future. We’ll have unstructured meetings each Wednesday from 18:00 to 20:00 (6p-8p) starting Jan 21st, with the fourth Wednesday of each month structured towards contribution towards a global challenge. The next such structured event will be on January 28th, on the subject of ethnic violence. You can see notes on this and potential future subjects here, and can register here.
About Ebola at NECSI [briefing by Yaneer]
NECSI has a history of studying Ebola models, and has predicted something similar to what is currently going on in West Africa for some time now. NECSI started with a model of pathogen evolution in which the most aggressive stable state has virus constantly passing slowly through populations, creating islands, dying out as people expand into areas with no disease.
Aggressive diseases plus long-range transport
Then if you add long-range transport, you get more and more aggressive strains. The more long-range transport you have the more aggressive the strain can be without dying out; and eventually could kill an entire global population. Paper published in 2006, mentions risk of Ebola.
As transportation becomes more pervasive, vulnerability increases.
Early warning and preparedness
Presented to the WHO in Jan ‘14. They were respectful and excited by the work. Discussed other public health issues faced by WHO, however didn’t return to pandemic models.
Since then: outbreak happened. Lots of discussion. Why don’t we engage in risks in a more serious way? Everyone thinks their prior experience indicates what will happen in the future.
- Look at past Ebola! It died down before going far, surely it won’t be bad in the future.
- Models of outbreaks look at existing conditions, which prove to be too limited here.
Example: with flu, people take exactly that disease and known circumstances, and simulate an outbreak, ignoring changes in the disease or in the conditions (and: nothing has to change in order to have huge risk). the same properties could remain, but a low-probability event could unfold, “fat tail distribution” – past experience isn’t necessarily a predictor of what will happen in the future.
Individual and community
Contract tracing, the standard public health method, doesn’t work well when there are more than just a few cases. Stop thinking about the contacts of the person, think about the community. Travel restrictions so new communities aren’t infected. Now that people go door to door for symptom screening, the cases have decreased dramatically in Liberia.
People were saying: “The beds are empty!” Authorities responded: “We can’t figure out why. We think people are still sick!” Why are the hospitals and authorities waiting for the sick to show up? Going door-to-door in the neighborhoods shows what’s going on, and is what is effective.
Once you know the right question, the answer is clear.
Interests
We then stated our interests – each person said one thing about the topic or intro talk they’d be interested in diving into more during breakout groups
Collective understanding, action
Educating people, also incentivizing doing the right global thing
Organizational Inertia – shifting mindsets
Look at reactions of the press
some people saying it’s foolish to talk about Ebola, it doesn’t cause enough deaths — measuring car accidents in the city reqs a small sample; to rule out ebola you need a larger sample.
Treating the community vs individual
Medical risks and questions
Question about door to door: hospitals can be a place for transmission; when you move door to door how does this spread?
Who goes door to door? (send teams. food, &c. they got neighborhood reps to do it)
Marshall / LBR implementer
Medical decision of how to respond
Interrelationships & measurement
Multidimensional; interrelated
Appreciating flexibility of complex analysis to provide new angles
How can we gauge effectiveness in real time? / control groups
General questions:
Building plans over time: how do we share understanding over time
Sharing practice across diseases
? what happens to ‘ECFs’ after the outbreak?
Breakout Groups
We then broke into small groups to continue speaking about these various aspects. The rough notes follow.
Collective Action
Medical response is an individual response.
Go to where the problem is. Impacting people at different stages. Less disruptive to do at a community level. Leaves people where they are and acknowledges that there’s a problem, with a beginning, a middle, an end. Fear is enormous, people begin to see what they might be able to do. 6 years of war isn’t just psychological, it’s structural. So when it goes to the community, it changes that abandonment. Shifting a system
Active demonstration of care. Not just “you have to go to the hospital.”
Have to give up crucially important cultural burial practices.
Close to social unrest in Spain because of the nurse with Ebola.
Treating it as a community problem lets you treat things better on an individual level.
A village in SLE had 7 RC volunteers killed. So who goes door to door? If it’s someone from the community who knows, that’s great. How do you get the communication out there? how do you convince people? how do you get the thermometers out there? There’s an emerging best practice, how do you get the supporting best practice tools out there?
Would opening up internet access to more than first responders be “good” in that peopel could communicate and self organize, or “bad” in that people would aggregate to the area with wifi for easier transmission?
How is media doing on this? If effective community response is about people having the sam idea of the problem, what would US fear-mongering media deal with this?
We live in an information junkie culture. Public health issue at the level of action.
Everything old is new again. We created our public health systems around Cholera, which is twice as infectious and terrible. But our additional systems and structures take us away from our roots.
Social democracies in Denmark, Sweden come out of the Cholera outbreak; the class warfare in England and Russia is in part because they didn’t figure it out.
Want to know how the communities had people going door to door
Burn down Alter incentives for mainstream media to get it right (even if they’re being sensationalist). PRI is doing it right. Build from that.
We need to learn from history
Medical
Vulnerability by transmission, what about transmission that can counter vulnerability?
Propagation of disease and information. Overlap with media issues.
Risk assessment from door-to-door, does it introduce a new transmission risk?
Are community level interventions only diagnostic, or also educational?
Given the dangers of connectivity, how do we exploit those dangers to expose them? Model for hostile agents to move place to place. Immunity at a
Good information and bad information. Effective and ineffective. How do we not just track the disease but the information about the disease? Door-to-door.
- Ask Lyre if the above covers all that should be brought back to the filed
- Get the word out: on the necessity of contact tracing
Interrelationships & measurement
How do we know the impact of door to door work? or the evaluation of a particular model?
- use confidence intervals. widely, to clarify what isn’t yet known.
- find data you can measure quickly everywhere; see what you can learn from them
- set up systems measuring this continuously; or on demand when risk rises
- find alternatives to controls (where traditional c. is immoral)
- (had a real control here: in opinions about how authoritative to be and act)
- define how [a place?] to set up and publish about such experiments
- it’s hard to measure where things start; focus on where thing are transmitted. that changes less over time.
- identify and track possible levers in this area
- Can’t observe causality. Could say, under model A it’s more likely that things went down because of change C.
- Be sure to include confidence intervals, not specific propbabilities
- find the parts of the system that don’t change.
- find where decisions have to be made, and which ones make a difference
- Need broad spectrum activity: you can’t simply test one action at a time, you are often hedging
- Trade-offs: problems with running a pure control. There’s risk aversion; morality; and uncertainty about how harmful both activity and inactivity would be.
Closeout
How to act?
- How do you get such a bound when statistics are small? Perhaps you only have 4 distinct outbreak regions.
- How do you know treatment regimes (social as well as medical) work?
- Are there moral ways to run a control? Looking into the past, before you applied it; or in regions where you can’t do it for some reason.
- find systemic shocks, other forced variation
- real-time understanding is still a problem
- reporting is complicated as well. who and what gathers data?
- find data feeds that can be gathered quickly (and learn ways to extract what you want from that sort of data)
- Try to iterate: to get enough statistics to say something meaningful
- Fever sensor (for flu) – can be used at a distance.
- How do you prevent it?
- YB and NT have written a paper saying it’s a fallacy
- you see a lot of false positives if you overfocus
Related past discussions
- Systemic v. idiosyncratic risk
- Lots of diseases that may come from Ebola (different imprint)
- Wei (from Hong Kong): Makes me think of swine flu.
- Even the govt didn’t really mention transmission; and people immediately started to cover themselves and put on masks.
- Distributed response and decision-making is possible
- There are things about disease that we can learn, so it’s clear how to react / how to avoid overreacting.
- Compare computational effects in finance. Similar distributions: fat-tailed. Don’t have the option to cut transportation (there: of data, here: of medical personnel)
- The # of pre-panics is monstrous. This is dealt with using circuit breakers.
- Consider creating similar circuit breakers. That’s the only way to avoid the fat tail.
 Final note on false positives (making people not take alerts seriously). Find a non-binary approach. “If X occurs here, it will be due to amplifying factor Y” — so you can target a response that way in each environment.
Final note on false positives (making people not take alerts seriously). Find a non-binary approach. “If X occurs here, it will be due to amplifying factor Y” — so you can target a response that way in each environment.
- We could know in W Africa: there’s a risk from having too few clinics & community centers.
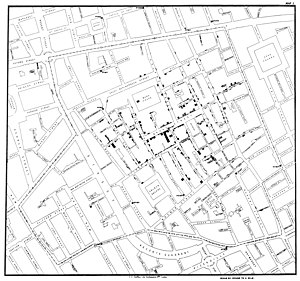
- Early disease: 1900s. John Snow knocked on doors to find cholera. Early crisis maps.
- We started a war with journalism over ebola: empiricism of the idiot: saying that more people X than die of ebola. overreaction irrational; we had to fight to say it is rational: panic, but early and in the right spot, not late and everywhere else.
- Think about framing the conversation when publishing to social media. Bypass the press, since they focus on naive issues. And set up a relationship for future communication
Reflection on the Salon’s Structure
Distribute info beforehand: compile readings, slides.
More flipcharts, sharpies, sticky notes. Up on the walls.
Not enough disagreements. Invite a journalist. Someone from other sides. A non-complexity person.
Invite more practitioners.
Return to the topic: revisit, learn, apply.
Multiple breakouts, idea transmission between them
Skepticism makes it easier to take decisive action? The more uncertainty there is overall, the more conservative.
We’re in a time of great risk. How do we respond?
Our current vulnerabilities are growing; without a better avenue for global response, we won’t survive. We have to build those mechanisms.
How do we engage with these problems, how do we discuss them?
How do we develop and propagate these ideas, and welcome more participants?
Expand the community engaged here. We dont need to coordinate a UN meeting to bring about global consequences.
Connected world. if we do stuff here, it can have global consequences.
Renew the way we tackle problems.
Ongoing structure
Once a month – targeted at doing something.
Weekly discussion → action. (what could be done, with whom, how to communicate?)
Rather than looking at one problem per week, look at one type of action per week and look at how it applies across problems.

Local community health approaches to ebola in Liberia http://t.co/jXk9ROnzNA
Pingback: Four short links: 6 January 2015 - O'Reilly Radar